Patient Information
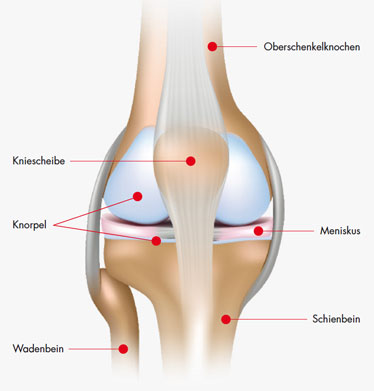
How does our knee work?
The knee is a hinge joint and the largest joint in the human body. Under normal use, the knee is often loaded with more than six times the body weight, and at the same time it must ensure sufficient mobility. The knee consists of two individual joints, the patellar joint (femoropatellar joint) and the actual knee joint (femorotibial joint). The thigh bone (femur), the tibia and the patella form the bony joint partners. For perfect gliding, the gliding surfaces of all joint partners are covered with a layer of cartilage. The menisci are located between the thigh and lower leg bones and increase the load-transferring surfaces of both joint partners.
.

Knee arthrosis
Knee arthrosis
Causes and symptoms
Knee joint arthrosis – also known as gonarthrosis – is a disease of the knee joint that often occurs in older people. It involves wear and tear of the cartilage surface of the femur and tibia, i.e. the cartilage layer that is supposed to protect the joint is destroyed and can no longer act as a shock absorber. The bones then rub directly against each other, they are worn out and can even deform.
What symptoms can occur?
- pain on exertion / starting pain in the morning
- Diminished walking distance
Main cause of arthrosis
The main cause of osteoarthritis is age and general wear and tear of the joints over the years.
Other risks
- osteoporosis (bone loss)
- overuse or overloading (e.g. in case of overweight)
- articular inflammation (e.g. due to rheumatic or metabolic disorders)
- accidents or injuries

Phsiotherapy for knee arthrosis
How is osteoarthritis best treated?
Complete healing of arthrosis is still not possible today. However, medicine offers proven treatment methods that are based on you as a patient and your state of health. Conservative treatment, i.e. without surgery, attempts to alleviate symptoms and improve mobility. If these therapies are unsuccessful, the insertion of an artificial joint can help to restore your quality of life.
What does a conservative treatment do?
There are different ways to treat the symptoms of knee arthrosis with conservative therapies.
This includes for example:
- Cold and
- Thermal applications
- Electrotherapeutic applications
- Orthopedic shoe insoles
- medicines for joint irritation
- Pain Therapies
- radiosynoviorthesis
- physiotherapy
- Food supplements
- Acupuncture
What can you do yourself
Discuss with your doctor whether a change in diet and/or weight loss can help your symptoms and joint. By arrangement, you can do light sports that are easy on the joints, such as water gymnastics. Also avoid a “relieving posture” in order to relieve the joint. This usually leads to further complications in the joint and ligaments. Special movement exercises should help you to cope better with everyday life. A professionally supervised physiotherapy can support you in this process.
The artificial knee joint
If only one more operation helps
Once all conservative options have been exhausted, your doctor will talk to you about surgery. The goal is to significantly improve your quality of life again. The implantation of artificial knee joints has a long history in medicine and is now one of the most common procedures. Implants, technologies and methods have been continuously developed since then.
How is an artificial knee joint constructed?
The artificial knee joint, also known as an endoprosthesis, consists of three parts: a femoral prosthesis (femoral component), a tibial prosthesis (tibial component) and the so-called inlay, which lies between the two parts as a sliding component. The femoral and tibial components of the artificial knee joint are usually made of cobalt-chrome alloys, while the sliding surface of the artificial joint is made of a special, very smooth and body-compatible plastic.
.
The artificial joint replaces the diseased parts of the joint that cause the discomfort through wear and tear. In the knee joint, usually only the diseased sliding surfaces of the joint are replaced. The femoral component for the thigh slides on a special plastic (polyethylene) that is fixed to the tibial component for the shin. All elements of an artificial knee joint work together in the same way as the natural joint. In the meantime, modern implants and surgical techniques are adapting more and more individually to the respective needs and circumstances of each patient and are intended to ensure pain-free mobility after arthrosis. For some years now, in addition to conventional joint replacement, patient-specific instrumentation has been used more and more. Here, special instruments are individually manufactured for your operation in order to be able to insert the optimal implant for you with an exact fit.
.
knee implants vary in shape, size and material depending on the clinical picture and stage of the disease. Depending on the situation or individual needs, the doctor can find the best solution for each individual patient.
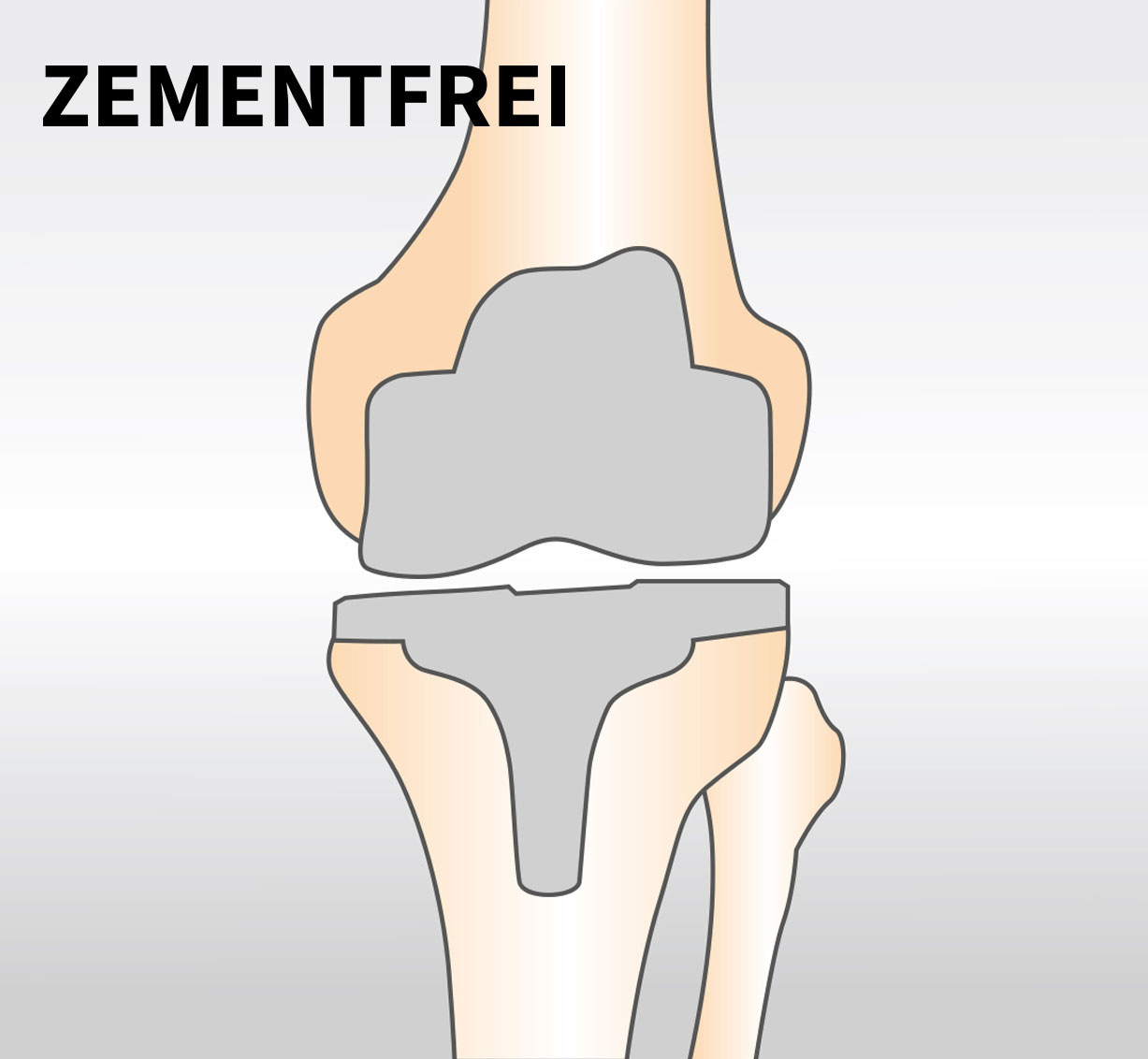
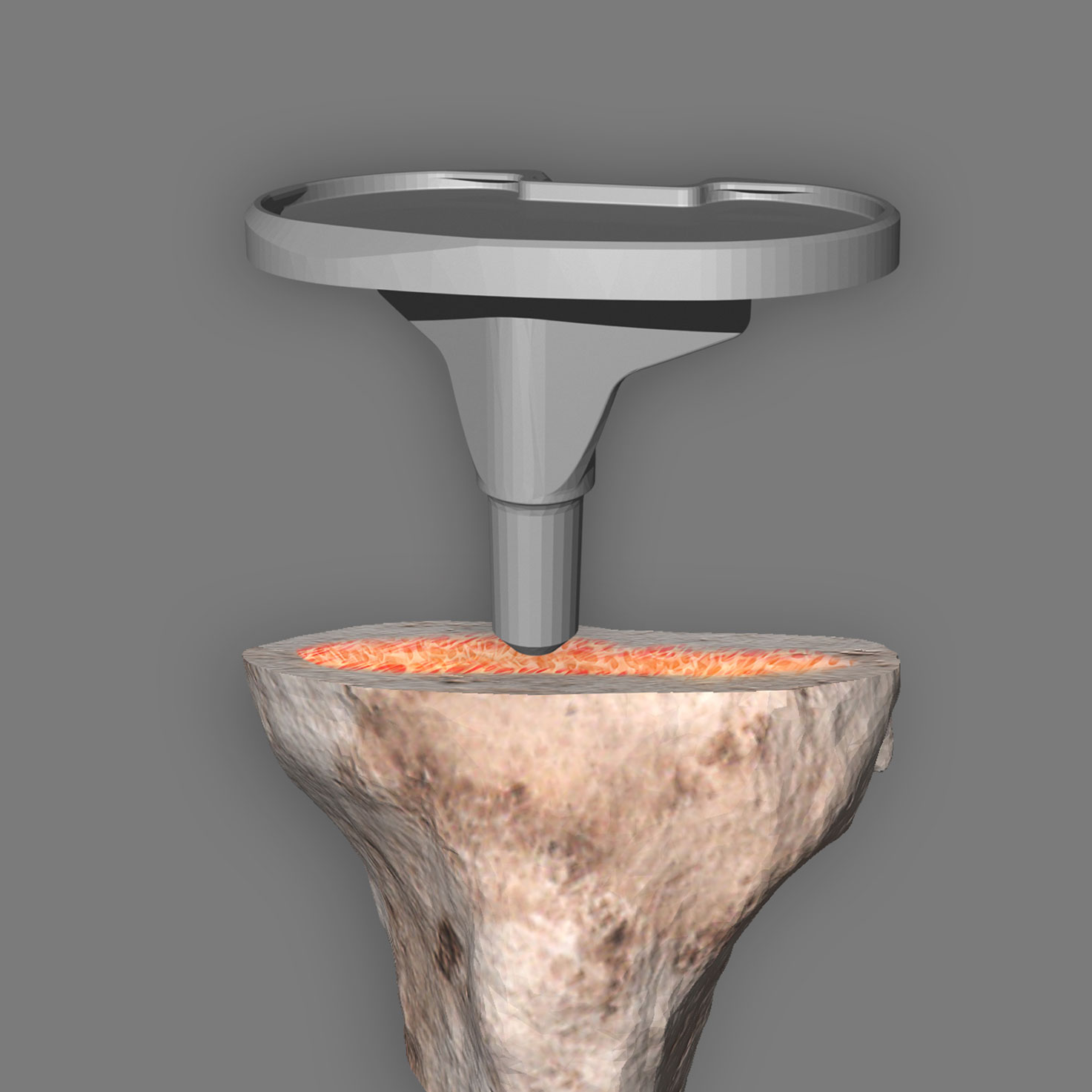
How is the prosthesis connected to the bone?
The principle of cementless anchoring is used for biological anchoring. This means that the implant surface is in direct contact with the bone and that biological healing/adhesion “osseointegration” occurs. The bone remains active, grows together with the knee prosthesis and forms a biological unit. The shape and surface of the implants are of decisive importance for cementless anchoring. Stable and permanent anchoring is a basic requirement for the durability of the artificial joint.
.
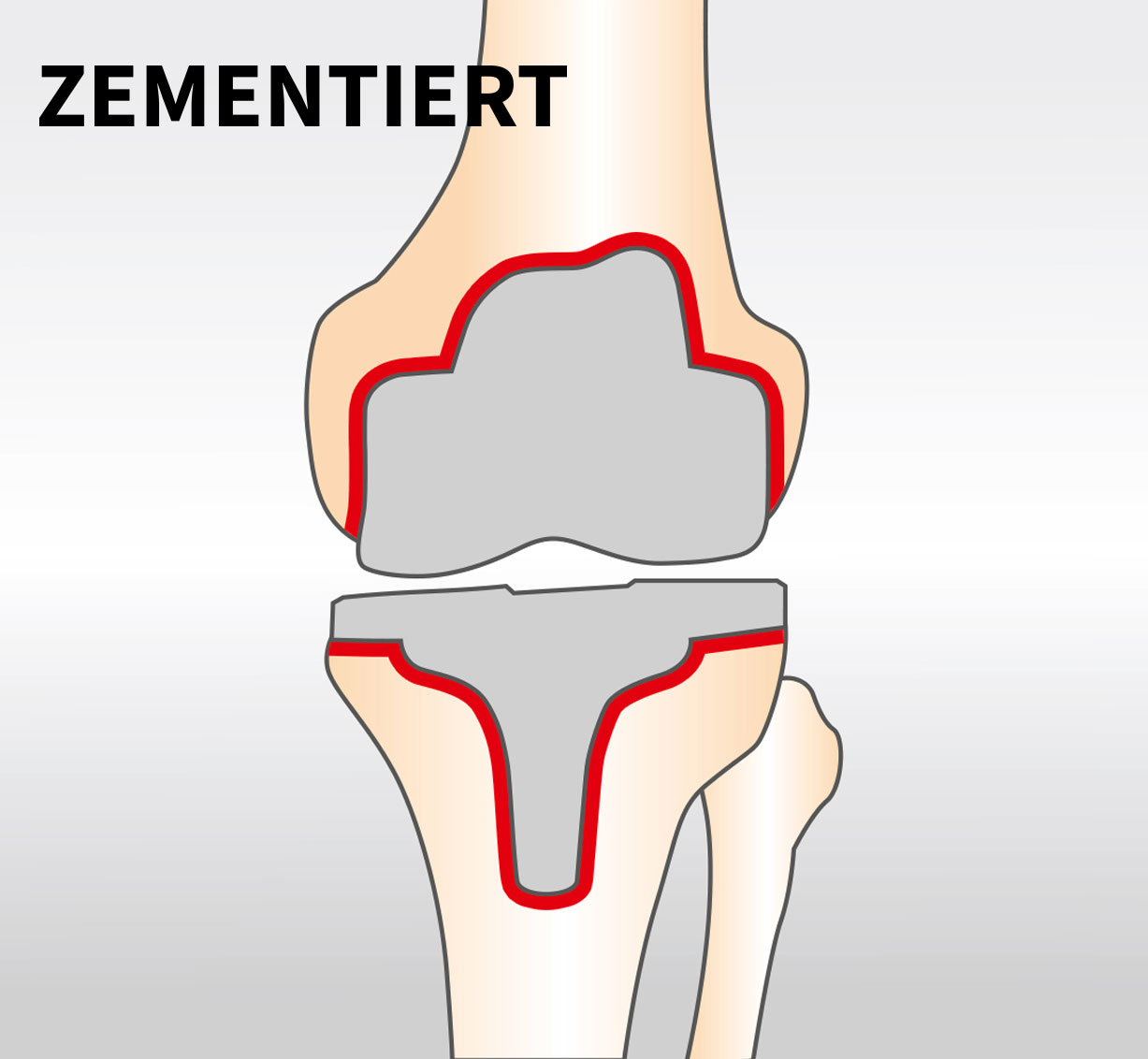
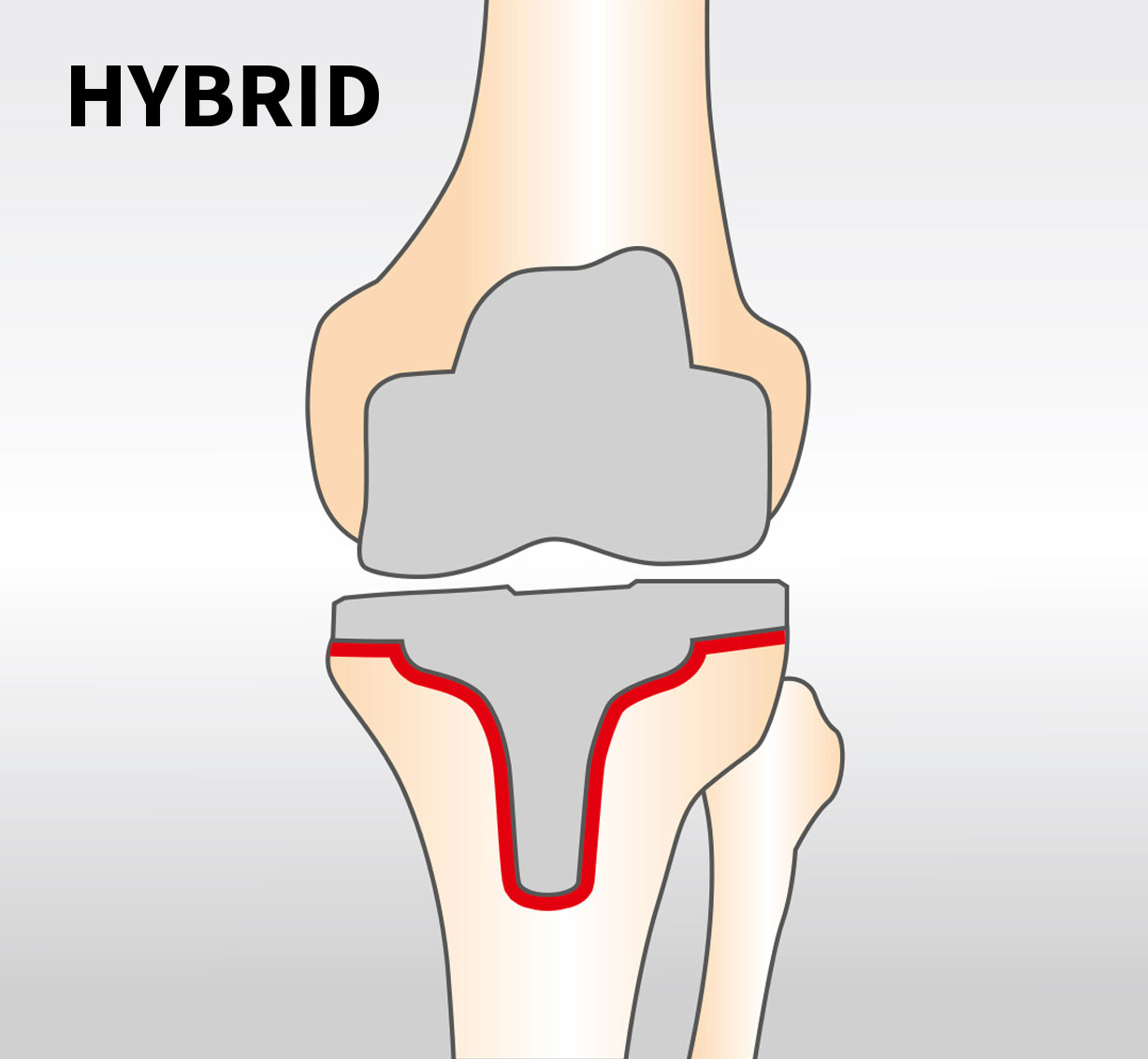
A variety of anchorage forms are used to firmly connect the implant to the bone. A distinction is made between cemented, hybrid and cementless prosthesis anchoring. In hybrid and cemented restorations, this is done with bone cement. In this case, the tibial component (hybrid anchoring) and in some cases also the femoral component (cemented anchoring) are connected to the bone by means of a fast-setting plastic (bone cement). This form of anchoring has reached maximum stability very quickly, shortly after the operation.
.
1. cemented anchoring
2. Hybrid anchoring
3. Cement-free anchoring

Scan
CT scan of your knee
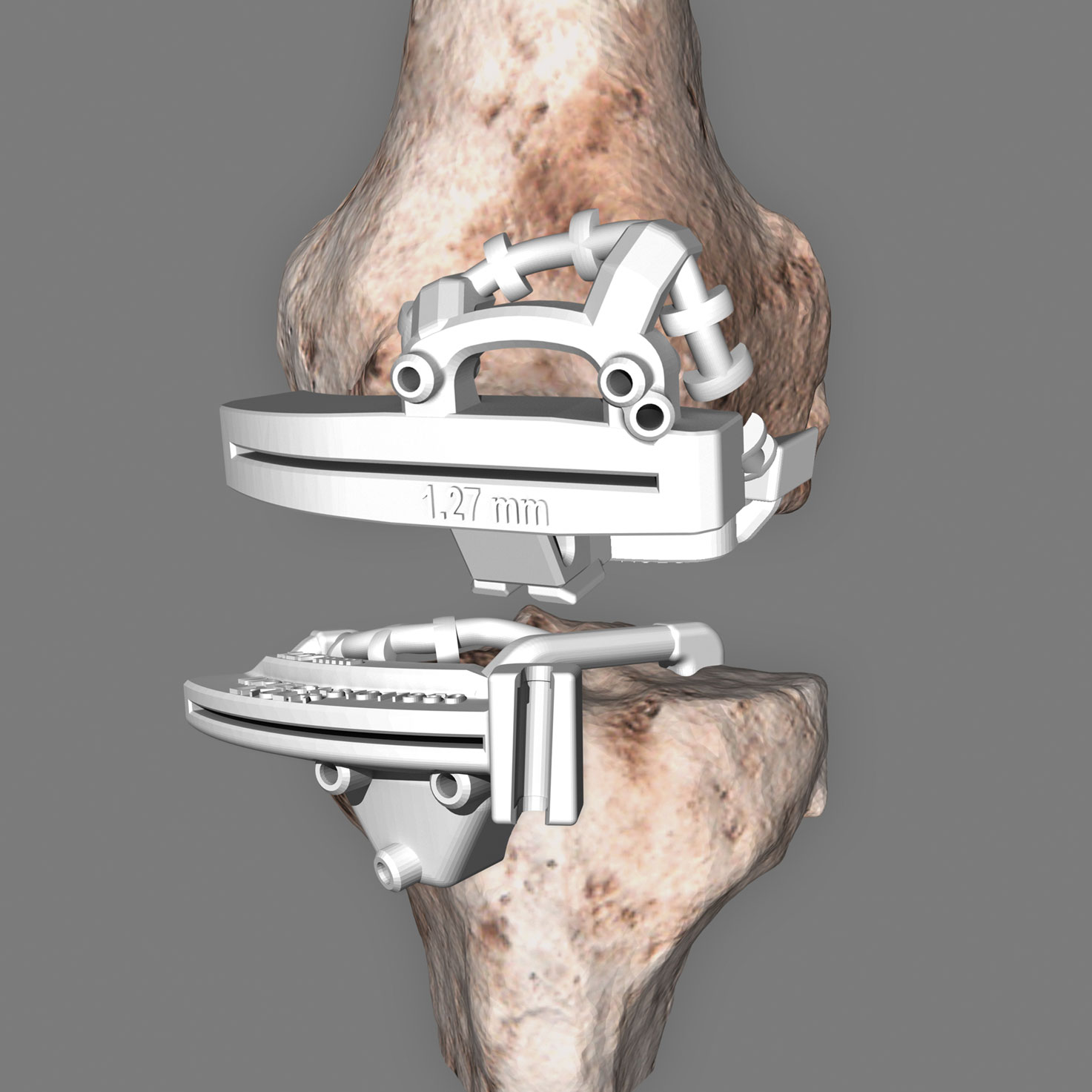
An interactive 3D web planning tool helps the surgeon to plan the operation individually. For this purpose he uses computer tomographic (CT) slice images of the knee, hip and ankle joint, and if necessary also x-rays of the whole leg.

Individual planning
Interactive three-dimensional CAD model of your knee and implant
The surgeon will then determine the ideal position of your implant for you. The implant and instruments provide your surgeon with customized support during the operation, during which your own bone substance is largely retained. This is important for the best possible stability.
Optimized surgical technique
Patient specific instruments
With 3D reconstruction and planning, your surgeon will need fewer steps during surgery, so the procedure can be performed in less time. For you, this means fewer anaesthetics that burden your body. Your muscles are not cut through, but only pushed aside. This allows the wound to heal faster later. Thanks to the three-dimensional model, the surgeon places your new knee joint precisely in the right place. The surgical instruments are also individually adapted using the 3D model and can only be placed in one position for a perfect fit. This enables the surgeon to implement the individually planned steps exactly during the operation. Alignment aids, for which the bone has to be reamed, are no longer required thanks to the 3D instruments. More bone substance is thus retained. The procedure is performed more gently and is associated with significantly lower risks (e.g. for embolisms).
What happens during the OP?
In order to match the knee joint perfectly to your personal bone structure, anatomy and needs, your doctor selects the appropriate femoral and tibial components. In the next step, the worn joint surfaces on the femur and tibia are precisely removed and the remaining bone is prepared for the implant. The bone is modeled so that the implant fits perfectly in its bony environment. Depending on the type of prosthesis used, the knee prosthesis is either cemented into the bone, inserted without cement or screwed into place. An extremely smooth and low-abrasion plastic sliding surface is then clicked into the tibial component. All three parts make up the new knee joint.
The operation at a glance
1. cutting blocks are placed on the thigh/lower leg bones
2. femoral component is inserted
3. Tibial component is used
4. The plastic inlay is clicked into the tibial component
5. Femoral and tibial components and plastic inlay form the new knee joint
What else can I do myself to optimally prepare for the operation?
Good fitness can help you get back on your feet faster. Talk to your doctor about the type and extent of your sporting activities. The better you are in shape, the faster your body can cope with the stresses of surgery. If you are overweight, now would be the right time to do something about it. Every missing gram that you can lose before the operation significantly reduces the stress on the new joint. Quitting smoking can also help you recover faster, so seriously consider quitting smoking. Knowledge relaxes and calms you. Therefore, please feel free to ask your doctor or the staff everything about your stay in hospital. If you have any questions about anesthesia, medication and nutrition, they will be happy to answer them.
Which form of anesthesia is suitable?
As a rule, admission to the hospital takes place the day before the planned operation. Usually your personal data will then be requested and you will be assigned to the ward and room. An anesthesiologist will then discuss the planned anesthesia with you. Today, artificial knee joints are used both under general anesthesia and with the help of spinal anesthesia.
Spinal anesthesia (partial anesthesia)
In this procedure, an anaesthetic is injected at the level of the lumbar spine to numb the lower half of the body.
General anesthesia (general anesthesia)
In general anesthesia the patient is put into an artificial sleep. Both the consciousness of the patient and his pain sensation are switched off.
What does "minimally invasive" mean?
Today, various minimally invasive procedures are available for knee joint implantation. The aim here is to use as little soft tissue as possible and to avoid damaging it. The advantages of a minimally invasive operation are
- Faster rehabilitation
- Reduced pain
- Hardly any blood loss during surgery
- No muscle injury or separation
What risks can occur?
In Germany alone, more than 160,000 knee prostheses are implanted annually. This makes the operation one of the most well-known treatment methods. However, as with all operations, knee joint implantation also involves risks.
This includes, for example:
- wear and material overload
- infections
- Restricted range of motion
- vascular/nerve damage
- incompatibilities
- bone fractures
- Loosening of implant components
- calcifications in the musculature
- thrombosis
- pain
What diagnostic procedures are available?
X-ray image (stationary)
The irradiation of body parts with X-rays is shown in images called radiographs or x-rays.
Magnetic Resonance Imaging (MRT)
MRI is an imaging procedure without radiation exposure that is used to visualize the structures and functions of tissues and organs.
Computer tomography (CT)
Computed tomography is a procedure for the layer-by-layer imaging of bone structures based on X-rays. The examination can be performed quickly and is very precise.
How long does a knee implant last?
Despite its high performance, an artificial joint is never equivalent to a healthy natural joint. In the scientific literature, the average risk of a replacement operation is given as a maximum of 1% per implantation year. Thus, many prostheses even last a lifetime. Causes for premature loosening of the artificial joint are, for example
- Infections
- Instability
- Bone quality
- Accompanying diseases/pain
- accompanying factors such as overweight
- too much or wrong load
- Broken bones
Can one react allergic to a prosthesis?
Please inform your doctor in advance about any allergies you may have. He will inform you about risks and alternatives. However, there are now very good material alternatives for potential allergy sufferers. Please also remember to bring your allergy passport and mention existing reactions to medication or latex.
What can I do directly before the operation?
Not only the doctor, but also you can contribute a lot to the success before and after the operation. Sometimes it is just the little things that can make your everyday life easier. Well prepared, your recovery after the operation can progress more quickly. You should think about some things and take precautions now.stock up on food. This will save you unnecessary shopping. If you are cooking, prepare larger portions now and freeze individual meals in small containers for later warming. Put all the things you use often on a height between your waist and shoulders, because in the first weeks you will be restricted in your freedom of movement.There are some aids that can help you in your everyday life after the surgery. For example a long shoehorn, for easier dressing of the shoes or a handle on the shower, for a safe entry and exit. Your clinic has a lot of experience with things that can make life easier after the operation. Talk to them calmly and they will certainly be able to give you valuable tips to take home.
Is there a checklist for the hospital visit?
Checkliste „Hospital stay“
- Health insurance card (if available)
- Letter of referral from the referring doctor
- Personal medicines
- Information on known allergies
- Contact addresses with telephone numbers of your contacts, friends & acquaintances
- Pyjamas/night shirts (unbuttonable)
- Walkers/Walking Sticks
- Care products (toothbrush, toothpaste, soap etc.)
- Jogging suit and/or bathrobe
- X-ray images, examination reports (if available)
- Sports shoes (if possible with velcro fastening)
- long shoehorn
- shoulder bag/backpack
- Some cash
When do follow-up appointments take place after the operation?
In consultation with your doctor, this should be done twice at 6-month intervals in the first year and once every two years thereafter. Please bring your last X-ray and the implant passport with you. Every follow-up check should be entered in the patient passport. This way you always have an overview. The regular check-ups allow possible complications to be detected very early. If severe pain suddenly occurs, the treating physician must be consulted immediately.
With your knee endoprosthesis you have a high-quality artificial joint with which you can achieve your desired quality of life again. With the right behavior and regular checks, you can assume that the joint will have a long life.
Can or should I do sports after the surgery?
Exercise and sports are not to be avoided in the first 6 months, but there are a few points to consider. After consultation/agreement with your doctor you can start using
start with sports.
Suitable sports
- hiking/walking
Constrained>/strong>
- swimming (backstroke and
Crawl)
Sports with high stress on the artificial joint (ball sports, as well as sports where there is a higher risk of falling) are less suitable. Cycling and especially e-biking is not recommended until a complete ability to react is restored. Extreme overloading leads to increased stress and wear on the prosthesis and reduces the life expectancy of an artificial joint. Ultimately, this can lead to premature loosening.